The features of the general practice/family medicine speciality in Europe include developing a person-centred approach. Dr Francisco Camarelles Guillem shares his experience with the challenges that General Practitioners (GP) have to face in their practice.
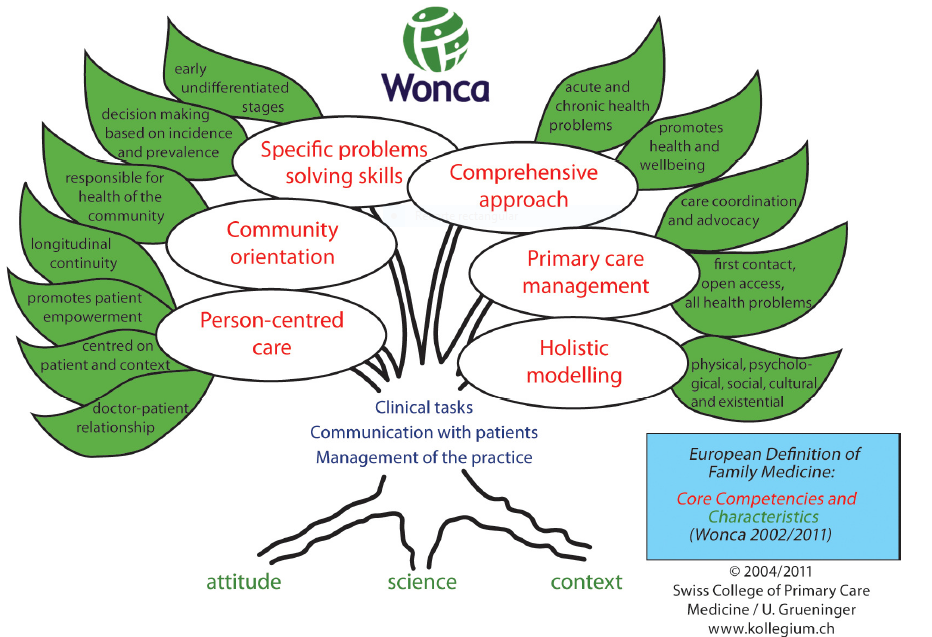
General practice is an academic and scientific specialisation with its own educational content, research, evidence base and clinical activity. It´s a clinical specialty that is based on primary care. The European definition of general practice by WONCA EUROPE (The European Society of General Practice/ Family Medicine) describes the key features of the discipline, and the role of the general practitioner (GP), as well as the core competencies of the GP. The features of our speciality include developing a patient-centred approach, orientated to individuals, their families and communities, and promoting patient empowerment.
For the past 25 years, I’ve been working as a GP in the Infanta Mercedes Primary Care Health Centre in Madrid, close to the Santiago Bernabeu Stadium of Real Madrid Football Club. To be honest, I don’t like football very much. As a GP, I deal with people and their problems in the context of their life circumstances. I don’t see them as the owners of impersonal pathologies or just “cases”. I think that the starting point of every health care process is the patient himself/herself. To understand the way a patient faces his/her health issue is as important as the dealing with the illness itself. Having been working for many years side by side with this patient’s dimension, my conclusion is that the common ground for all of us should be each person’s beliefs, fear, needs and expectations, in order to be not only more successful but also to perform better as humans.
Promoting patient empowerment in a primary care centre
Most of my patients lack self-care, that means they don’t know how to stick to life behaviours in favour of their own health in order to reach a well-being level that can be considered optimal. Another problem is having low health literacy, the degree to which people have the ability to obtain, process and understand basic information about their health and health services, in order to make appropriate decisions. Both are very important in people’s health.
As a GP I may be holding a strategic position when it comes to promote patient empowerment and self-management in my daily clinical practice. In my view, the starting points for a continuous educational process are both the multidisciplinary approach, the strong relationship based on a unique consultation process and the trust between the health care professional and the patient. That’s how we will be able to empower our patients, by knowing that the three key dimensions of patient empowerment are health literacy, self-care and shared decision-making.

Dr Francisco Camarelles Guillem
Francisco works as a General Practitioner in Madrid and he is interested in Preventive Activities and Health Promotion. He is a member of the Spanish Society of Family and Community Medicine (semFYC). semFYC is a featured member of WONCA EUROPE (The European Society of General Practice/ Family Medicine).
The challenges of shared decision-making and patient activation
Two main challenges I have to face in my daily business as a GP are the shared decision-making process and the patient “activation” procedure. As for the first one, when it comes to making decisions, it is crucial that the conversation between doctors and patients is as honest as possible, and that both parties realise they are involved into a thinking, feeling and discussing about a situation which will have consequences on both sides. On the other hand, activating my patients in they self-care is not so easy. Patient’s activation is related to knowledge, skills and confidence, so each one can manage his or her own health.
We know what strategies are used by health professionals who are good “activators” of the change in health behaviour of their patients. Mainly, there are five strategies which have been proven most successful in enabling patients to change their lifestyle: emphasizing patient responsibility, collaborating with patients, identifying small steps towards change, scheduling frequent follow-ups, and showing interest.
It is also interesting to know which less successful strategies are being used by other professionals. Highlighting those descriptions of the negative health outcomes to be expected if unhealthy behaviours are not faced: “If you do not stop drinking alcohol, your liver will end up having a cirrhosis disease.”




