
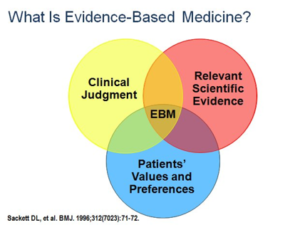
Evidence-Based Medicine (EBM) is the integration of best research evidence with clinical expertise and patient values. Since its first definition, there has been an increasing emphasis on the limitations of using evidence alone to make decisions, and the importance of the values and preference. In healthcare decision making, values and preferences refer to the internal processes that individuals use when balancing potential benefits and harms derived from treatment.
Patients’ values and preferences and decision-making
 The integration of patients’ values and preferences can be considered an ethical mandate since patients are affected by the different healthcare decisions, including clinical recommendations. From a policymaker perspective, the evidence informing about patients’ values and preferences can help to delineate more patient-centred programs; and from a healthcare practitioner perspective, this evidence can help the process of decision-making in clinical encounters.
The integration of patients’ values and preferences can be considered an ethical mandate since patients are affected by the different healthcare decisions, including clinical recommendations. From a policymaker perspective, the evidence informing about patients’ values and preferences can help to delineate more patient-centred programs; and from a healthcare practitioner perspective, this evidence can help the process of decision-making in clinical encounters.
Patients’ preferences are the result of experiences, expectations and attitudes towards health and disease. Evidence informing values and preferences is particularly critical in scenarios with scarce or low certainty of the evidence of effects; when it is necessary to make explicit these usually invisible aspects. There are diverse methods to obtain patients’ values and preferences, and these include both quantitative and qualitative research.

Ena Niño de Guzman
As a healthcare researcher, Ena is part of the Sant Pau team of COMPAR-EU. She leads the development of the work that will inform about the patient perspective throughout the project. Her PhD project is based on this work. She was recently awarded a Rio Hortega investigator contract by the Instituto de Salud Carlos III (Spanish Ministry of Health).
The patient perspective in self-management interventions
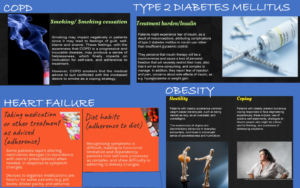 The COMPAR-EU project aims to identify the most effective and cost-effective self-management (SM) interventions for patients living with one of four high priority chronic conditions (type-2 diabetes mellitus (T2DM), obesity, heart failure, and chronic obstructive pulmonary disease (COPD)).
The COMPAR-EU project aims to identify the most effective and cost-effective self-management (SM) interventions for patients living with one of four high priority chronic conditions (type-2 diabetes mellitus (T2DM), obesity, heart failure, and chronic obstructive pulmonary disease (COPD)).
As part of COMPAR-EU, we have conducted a scoping review of quantitative and qualitative reviews to explore values and preferences of patients regarding the role of self-management in these conditions. This work was part of the development process of four Core Outcome Sets (COS), defined as a standardised collection of outcomes which should be measured and reported at a minimum in all trials of a specific condition or a trial population. The objective was to identify which outcomes emerged from the available published research evidence. We analysed the main findings of selected reviews and identified common themes related with potential outcomes of interest when dealing with SM interventions, and developed infographics to facilitate the discussion between patients, caregivers, and researchers participating in the consensus workshop of the selection of the COS.
In COMPAR-EU we are now conducting four overviews of reviews of studies exploring patients’ values and preferences, to collect and summarise the patients’ perspectives with one of these four chronic conditions regarding SM interventions. In these overviews, our focus will be to summarise how patients value the importance of outcomes, and the factors that might influence achieving the expected goals of SM interventions. We will provide summaries of findings to inform the different decision-making tools that will be developed in COMPAR-EU. More specifically, we will explore the extent of the certainty and variability in how patients value the importance of outcomes. We will also obtain relevant information regarding contextual factors that have an impact on the acceptability and feasibility of SM interventions. Some of these findings will help to delineate implementation strategies for SM interventions.

